How to recognize and refer children with hemiplegic (unilateral) cerebral palsy
© Lindsey Griffith, Betty Yundt, Darcy Fehlings, Peter Rosenbaum, 2013
What is cerebral palsy?
Cerebral palsy, or CP, refers to a group of developmental conditions that have several features in common. All are caused by some kind of injury to the developing brain. The injury can occur in the womb, during the birth of the baby, or in the first couple of years after birth. Common risk factors for CP include prematurity, low birth weight, multiple gestation, and infection.1
1
400
individuals in Canada are diagnosed with Cerebral Palsy (CP)
In Canada CP affects 1 in every 400 individuals and is the most common physical disability in children. The hallmark disability for individuals with CP is related to motor function – how a person develops and maintains control of their movement. Children with CP almost always have issues with whole-body movement, including walking, and often in using their hands and arms. In addition, they may also have other challenges resulting from their brain injury, including problems with seizures, learning, communicating, vision and hearing, and behaviour.
What is hemiplegic or unilateral CP?
33-39
%
of children diagnosed with Cerebral Palsy have hemiplegic CP.

‘Hemiplegia’, ‘hemiparesis’, or ‘unilateral’ CP affects the movement and muscle tone on one side of the body, although often the other side of the body may be affected to a lesser extent.2 It is the most common form of CP, with estimates ranging from 33-39% of all people with CP.3,4 A ‘stroke’ in the time before, during or after birth is the most common cause of hemiplegic CP. Multiple factors may interact to block the blood vessels in the brain and cause a stroke. Many times the cause of the stroke will never be known.5 As one side of the brain is injured, the opposite side of the body is affected; this can result in weakness of an arm, leg, or both on one side of the body. Sixty percent of children with hemiplegic CP have seizures in the newborn period.
What are the early signs of hemiplegic CP?
Hemiplegic CP frequently presents in the first year of life when parents notice a hand preference, which is very unusual in children at this age. Other signs include fisting of one hand and flexion (bending) of the elbow on the affected side. In supported standing, the child may stand flatfooted on their more functional side and up on the toes of the hemiplegic side. Likewise, the child may not bear weight well through the affected hand or foot. Some asymmetry in function might be noted when the child is crawling or attempting other motor activities and as a result the child’s crawling is often delayed.
For children under the age of 18 months, some ‘red flags’ include:
- Favouring one hand, leaving the other hand in a fist or reaching across their body to grab objects, or not bringing both hands together during play
- Delays in early motor milestones – rolling, sitting, pulling to stand, crawling, and walking
- Stiffness or weakness in muscles on one side of the body
- Difficulty with the early development of walking and balance
- Asymmetrical movement and posture
How is hemiplegic CP diagnosed?
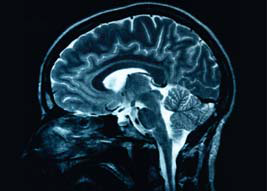
Hemiplegia is a condition best recognized by the story the parents tell and the observations we make when watching children in action. An MRI (magnetic resonance imaging) brain scan is the preferred method of neuroimaging for CP.3 MRI is useful for identifying the presence and location of a brain injury in almost 90% of children with CP.6 Children with hemiplegia commonly have abnormal cranial ultrasounds.
What is the outlook for children with hemiplegic CP?
The gross motor function of 88% of children with hemiplegia is classified as GMFCS level 1.7
This means that almost all children with hemiplegia can walk by 2 years of age without assistive devices, and by age 6 can:
- Walk long distances outdoors and on uneven surfaces
- Move from the floor or a chair to standing without using their hands for support
- Go up and down stairs without needing to hold the handrail
- Are beginning to run and jump.
Some potential challenges include:
- Difficulties with voluntary movement in one arm, for instance difficulty opening their hand, picking up small objects, turning the hand over. In the leg, there may be toe walking on the one side which can cause tripping.
- Increased muscle tone or stiffness in the elbow, wrist, knee, and/or ankle. The increased muscle tone may be more obvious when the child is running.
- Possible visual field defect or sensory loss on one side.
- Epilepsy can occur in 40-67% of children with hemiplegia, presenting later in life.8
- There may be some differences in sideto-side bone lengths and diameters which increase with age.9 This difference in limb length is usually not problematic for the individual with hemiplegic CP.
What should be done if concerns arise?
Refer to an early intervention program (occupational therapy and physiotherapy) and a pediatric developmental specialist or neurologist for further testing.
**Early intervention services, including therapy consultation, can be initiated before a formal diagnosis of CP is made.**
Case scenario
- Oliver is in the office with his mother for his 18 month well baby exam.
- Oliver’s general health has been good. He was born after an unremarkable pregnancy and delivery at 40 weeks gestation.
- His mother reports that Oliver is developing well and she has answered yes for all the questions on the 18 month Nipissing chart! He has been walking independently from 15 months, and he is starting to feed himself with his right hand. She does note that he has always preferred to use his right hand to play with toys, but she is not concerned as most people in her family are right handed. He is able to identify 3 body parts and has 10 words that he is able to use consistently. He enjoys looking at books and pointing to pictures.
- Growth chart indicates that Oliver is growing well. On observation, you wonder if he has mild increased muscle tone in the muscles that bend his left elbow but you are not convinced. You do note Oliver always uses his right hand when grabbing a toy. When he is standing he occasionally goes up on his left toe.
- Although Oliver is reaching many of his developmental milestones you are concerned about his right hand preference as you know children shouldn’t show a strong hand preference until well after 18 months.
- You refer him for a consultation and an MRI reveals evidence that he had a stroke as an infant. A diagnosis of Left Hemiplegic Cerebral Palsy is made.
- You have already initiated a referral for occupational therapy and physiotherapy consultations.
Typical milestones at 18 months
Gross motor (whole body) skills:
- Walks alone/moves about house without adult assistance
- Walks up stairs while holding on with one hand
- Pushes a toy while walking forward
Fine Motor (hand) skills:
- Uses both hands equally well
- Feeds self with spoon with little spilling
- Drinks from a cup
- Uses a pincer grasp
- Points using pointer finger
- Can build a tower of two to four blocks
When to be concerned
At 18 months, be suspicious of problems in motor development if one or more of:
- Not yet walking
- Asymmetric movement or posture
- Isolated toe walking
- Walking with a wide base of support
- Established hand preference (hand preference should not be present before 18 months)10
For more information, please contact Peter Rosenbaum at canchild@mcmaster.ca.
